Daijiworld Media Network – New Delhi
New Delhi, Jan 17: A landmark global study published in the journal Nature has suggested that several psychiatric disorders share common genetic roots, raising the possibility that many mental health conditions may not need to be treated as entirely separate illnesses.
The research, which analysed psychiatric and genetic data of over one million patients diagnosed with mental disorders and nearly five million people without such diagnoses, found significant genetic overlap among 14 major psychiatric conditions. Scientists said the findings could pave the way for more effective, biology-driven treatment approaches and reduce the burden of multiple diagnoses and medications on patients.
According to the study, psychiatric disorders broadly fall into five genetic clusters — substance use disorders; internalising conditions such as depression, anxiety and post-traumatic stress disorder; neurodevelopmental conditions like autism and ADHD; compulsive disorders including anorexia nervosa, Tourette’s syndrome and obsessive-compulsive disorder; and a fifth category encompassing bipolar disorder and schizophrenia. Notably, bipolar disorder and schizophrenia were found to share nearly 70 per cent of their genetic drivers.
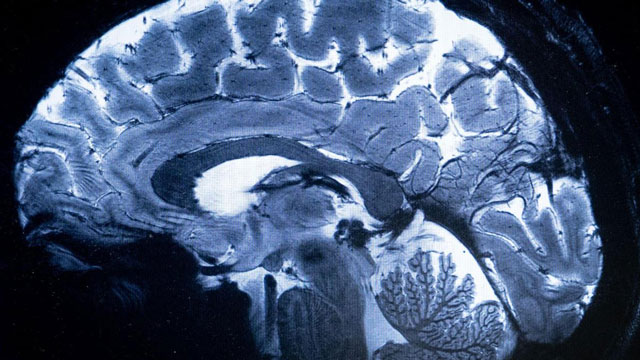
Researchers identified 238 genetic variants common across the disorders studied, many of which influence brain functions. A significant genetic “hot spot” was found on Chromosome 11, which contains genes linked to multiple psychiatric conditions. One such gene, DRD2, is a primary target of antipsychotic medications and plays a key role in dopamine regulation.
Experts said the findings challenge the long-standing practice of diagnosing psychiatric illnesses purely based on observed behaviour. “Genetics suggests these categories are more closely related at a biological level than we previously believed,” said study author Jordan Smoller of Mass General Brigham’s Center for Precision Psychiatry.
The study also highlighted why certain medications, such as antidepressants, are effective across multiple conditions. However, researchers cautioned that genes interact with environmental factors such as stress, upbringing and life events, meaning genetics alone cannot explain mental illness.
While experts welcomed the study as a major step forward, some noted that its clinical application remains limited for now. Mental health professionals said it may take years before genetic insights are incorporated into diagnostic manuals like the DSM, which guides psychiatric diagnosis worldwide.
Researchers also acknowledged limitations, particularly the lack of genetic data from non-European populations, and stressed the need for more diverse studies.
Despite these challenges, experts believe the findings signal a future shift toward biologically informed psychiatry, potentially transforming diagnosis and treatment over the next decade.